The Pelvic Floor's Crucial Role During Vaginal Birth and How to Support It
The pelvic floor has many roles in the body for such a small muscle group. However, one of those roles tends to be generally misunderstood. This is what the pelvic floor does during a vaginal birth.
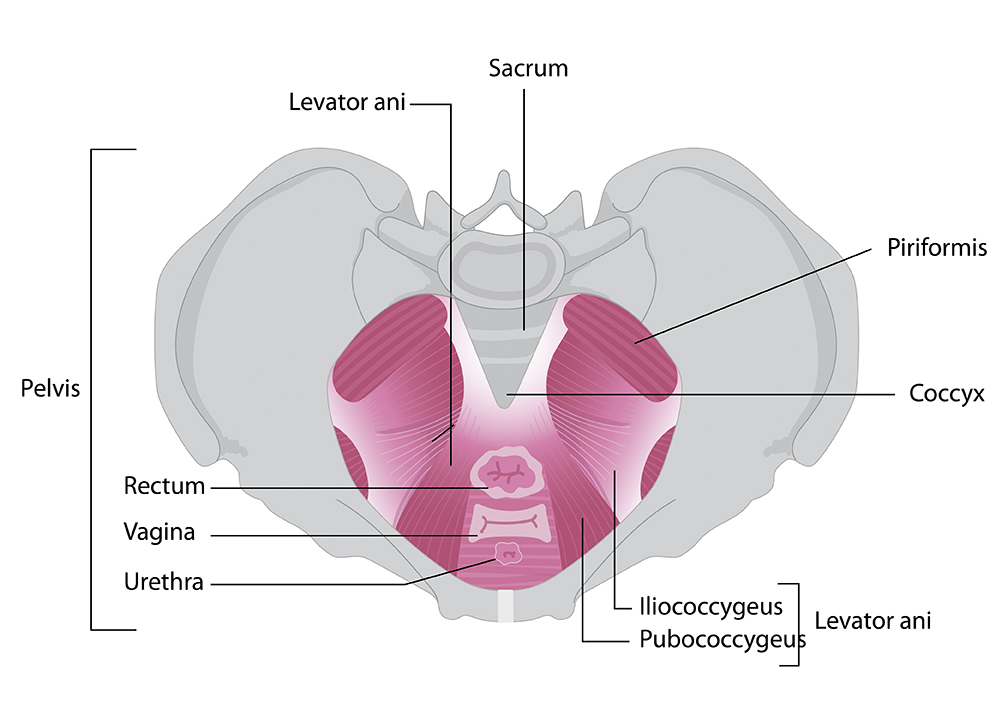
Let’s consider the anatomy of the pelvic floor before we dive into it’s role during birth.
The pelvic floor is made up of muscles, connective tissue and ligaments attached to bones. The front of the pelvic floor attaches to the pubic bones, the back attaches to the tailbone and the sides attach to the ischial tuberosities (sit bones). Effectively closing off the bottom ring of the pelvis. This configuration is to create a hammock of support for the pelvic organs and stability to the pelvic joints, while balancing internal pressure with the respiratory diaphragm and abdominal muscles.
©Expecting Pelvic Health
The uterus is one of the pelvic organs (even though it becomes an abdominal organ after the second trimester) and thus is supported by these tissues. The vagina ends at the introitus (the vaginal opening) which runs through the pelvic floor muscles.
©Expecting Pelvic Health
During birth the uterus contracts to expel baby through the vagina and out the introitus. Also during birth the joints of the pelvis widen and the bones shift to accommodate baby moving through the pelvis.
Since the pelvic floor surrounds the vagina and attaches to the bones that are meant to widen, the role of the pelvic floor during birth is to LENGTHEN.
Essentially, the pelvic floor needs to get out of the way of the baby by stretching 3-4 times it’s original length. This is critical for proper movement of the tailbone and sacrum to tip and also move out of the way. If there is any tension or tissue restrictions in the pelvic floor that prevents proper lengthening from happening baby position can be impacted, you may experience a longer labor, medical interventions may be suggested such as forceps or vacuum and you increase your risk of tearing/pelvic floor injury.
The good news is there are steps you can take to influence how your pelvic floor lengthens during a vaginal birth.
Assess your pelvic floor tone
Tone means the suppleness of the muscles and tissues. The best way to do this is by inserting your finger vaginally and seeing how soft or hard your muscles feel. Ideally your pelvic floor feels in between, not too soft and not too hard, with the ability to relax to your touch and contract on demand.
I recommend seeing a Pelvic Physical Therapist for the most accurate assessment of your pelvic floor, as we are trained to know what muscles and connective tissue are suppose to feel like and then can provide treatment to address any findings that may impact your pelvic floor fulfilling it’s role in birth.
You can also download my free Pelvic Floor Self Assessment Guide to learn more.
Assess your ability to lengthen the pelvic floor
It’s not enough to have ideal tone, but you also need to be able to consciously lengthen the pelvic floor. This is not only important for pushing a baby out, but for daily function like going to the bathroom.
The most direct way to assess this is while you are assessing your tone, seeing if you can actively bear down with the pelvic floor while inhaling. Imagine you have a tampon in and you want to slowly slide it out by moving your pelvic floor out to. If this is hard to do, then you either have too much tone or tension in the pelvic floor muscles to lengthen or you need to practice letting go.
Address the high tone or tension
You’ll want to release any tension or high tone in the muscles to promote lengthening. There are several strategies to do this with the most direct being manual massage and stretching of the pelvic floor muscles vaginally. Again, seeing a Pelvic PT is a great way to provide you with the individual guidance you need.
Vaginal massage of the pelvic floor requires insertion of a finger or a tool called a wand to gently hold and stretch the muscles as well as sweep from front to back. Both of these techniques are similar to what you may do to tight neck muscles. You want to be in a comfortable position to begin and as you become more adept at the releases change your positions to see if your pelvic floor responds differently.
You can also watch my video, Pelvic Floor Massage to begin.
Another way you can release tension in the pelvic floor is externally using tools like a rolled towel or ball. Since your pelvic floor is at the bottom of your pelvis, sitting on a towel or ball can help you feel and let go of tension. Watch this video for more guidance.
Practice positions that lengthen the pelvic floor
Lastly, using gently stretches and yoga positions that influence pelvis position can impact your pelvic floor. Doing stretches like cat/cow tip your pelvis back and forth which in turn changes your sacrum and tailbone position. Adding hip internal rotation by sliding your feet away from midline and turning your hip in opens the bottom of the pelvis even more. This is a great way to stretch the back portion of the pelvic floor that attaches to the tailbone. Find ways to incorporate hip internal rotation into comfortable stretches like sitting in W-sit on a block or cushion. Or sitting in wide leg and turning your legs in and out.
In addition to the stretches, resting or holding in positions that length the pelvic floor and breathing into the pelvic floor can improve your brain-muscle connection. Plus, you can assess your ability to ease into any tension or discomfort. Every little bits helps you connect to the pelvic floor, improving your chances of a helping the pelvic floor fulfills it’s role in birth.
For best outcome you’ll want to begin this process in your second trimester to see if you have tension/high tone or the inability to lengthen the pelvic floor. Then do the releases and exercises on a regular basis in your third trimester, starting no later than 36 weeks.
Hopefully by the end of this you understand that your pelvic floor is not meant to contract during birth. It’s main role in birth is the LENGTHEN, allowing the bones to widen and get out of the way for baby. Having a greater understanding of your pelvic floor prior to birth can improve your birth outcome by reducing risk of medical intervention and injury.
Ready to feel confident and prepared for your upcoming birth? I've created the Gentle Birth Guide—a step-by-step roadmap based on what I personally did and what I recommend to my patients to help them prepare for a smoother, more empowered birth experience. You can download this guide now and take the first step toward a gentler birth!